Botulinum Toxin Treatments: Uses, Safety, and What to Expect
Understanding Botulinum Toxin: Mechanism, Relevance, and Outline
Botulinum toxin treatments sit at the intersection of science and everyday confidence. They’re widely chosen by people who want to soften lines formed by repeated expression and, in many cases, to manage specific medical conditions driven by overactive muscles or glands. Their relevance has grown because outcomes can be precise and adjustable, downtime is typically brief, and results are temporary, making them easier to trial without a long-term commitment. In a world of bold claims, botulinum toxin offers something more grounded: a pharmacologic mechanism with decades of study, measurable endpoints, and a clear safety framework when used by trained clinicians.
At a cellular level, purified botulinum toxin works by blocking the release of acetylcholine at the neuromuscular junction. By tempering this chemical signal, the targeted muscle relaxes; when that muscle is responsible for expression lines, the skin can appear smoother. The same principle applies to glands influenced by cholinergic signaling, such as sweat glands in the underarm. Onset is not instantaneous: many people see first changes at 3–5 days, peak effect near two weeks, and a gradual fade over 3–4 months. These are typical timelines, not guarantees, because metabolism, dose, injection placement, and individual biology matter. Different commercial preparations of botulinum toxin exist; their units are not interchangeable, and clinicians select products based on training, goals, and regulatory availability in their region.
Beyond cosmetics, botulinum toxin is used in neurology, dermatology, ophthalmology, rehabilitation medicine, and urology. Examples include management of chronic migraine, cervical dystonia, eyelid spasms, limb spasticity following stroke, excessive underarm sweating, and overactive bladder symptoms in selected patients. In many countries, some of these uses are formally approved; others may be considered off-label based on clinician judgment and local guidance. The common theme is targeted, reversible modulation of overactivity—like turning down a dimmer rather than switching off the lights.
To help you navigate, here is the outline of what follows and how each section builds on the last:
– Aesthetic applications: where injections are used on the face, what realistic results look like, and how toxin differs from fillers and devices.
– Medical applications: which conditions may benefit, what outcomes are measured, and how frequency and dosing strategies are set.
– Safety and candidacy: side effects, contraindications, risk reduction, and how to choose a qualified provider.
– The treatment journey: consultation, procedure day, aftercare, timelines, costs, and long-term planning.
Aesthetic Applications: Areas, Expectations, and Comparisons
When people think of botulinum toxin cosmetically, they often picture smoother skin across expressive areas of the face. The most commonly treated zones include the glabellar complex between the eyebrows, the horizontal lines of the forehead, and lines radiating from the outer corners of the eyes. Other carefully selected sites may include the bunny lines at the bridge of the nose, a gummy smile from upper lip elevation, downturned mouth corners related to depressor muscle pull, and the masseter muscles along the jaw for contour refinement. The guiding principle is to relax specific muscles in a way that softens creases without flattening your natural expression.
Results develop gradually. Early changes typically appear within several days as movement becomes more controlled, with a clearer cosmetic effect by two weeks. The goal is harmony, not rigidity. If you imagine the face as an orchestra, botulinum toxin is like a thoughtful conductor, asking a few instruments to play more quietly so the whole piece sounds balanced. Treatments can be tailored for a very light touch—sometimes called “baby” or “micro” dosing—when maintaining full range of expression is a high priority. Conversely, moderate dosing can emphasize line softening in deeply etched areas, paired with follow-up reviews to fine-tune.
It helps to compare toxin with other options to set expectations:
– Versus dermal fillers: Toxin reduces motion-driven lines by targeting muscle activity; fillers replace lost volume or sharpen contours. They often complement each other but address different issues.
– Versus skincare: Daily sunscreen, retinoids, and moisturizers improve texture, tone, and collagen support, but they do not significantly quiet muscle movement; toxin does.
– Versus energy-based devices: Lasers and microneedling remodel the superficial and mid-dermal layers to improve texture and pigment; toxin acts deeper, at the neuromuscular junction.
Not everyone is an ideal candidate for every facial area. People with very heavy eyelids may not be suited to aggressive forehead relaxation because the forehead helps lift the brows; a conservative approach lowers the risk of a heavy feeling. Those with asymmetric movement may require customized patterns to avoid amplifying imbalance. A qualified clinician will observe your expressions at rest and in motion, map the relevant muscles, and discuss trade-offs openly. Maintenance is typically every 3–4 months, though intervals vary. Photographs taken before and about two weeks after treatment can be a useful record—not to chase perfection, but to confirm you are moving toward the look you want.
Medical Applications: From Overactivity to Measurable Relief
The same mechanism that quiets expressive lines can help calm muscles and glands that are working overtime. In chronic migraine, protocols in select patients use scheduled treatment across multiple head and neck sites at intervals of roughly 12 weeks, aiming to reduce the number of headache days. In cervical dystonia, targeted injections can lessen torticollis, neck pain, and abnormal head posture. Ophthalmology uses include blepharospasm, where excessive eyelid closures interfere with daily life, and strabismus in specific cases. Rehabilitation teams use botulinum toxin to address focal spasticity after stroke or in cerebral palsy, improving comfort, care, and in some instances, function alongside therapy.
Dermatology and autonomic conditions offer further examples. For primary axillary hyperhidrosis, injections reduce sweat production by modulating cholinergic input to glands; many patients report improved quality of life and wardrobe freedom. In urology, carefully administered intradetrusor injections for appropriate candidates can decrease urgency and frequency associated with overactive bladder. Sialorrhea, or problematic drooling, may be reduced by treating salivary glands under guidance. Bruxism and masseteric hypertrophy can sometimes be managed with jaw muscle injections when bite-related strategies alone fall short, though dental evaluation remains essential.
Outcome measures vary by condition:
– Headache disorders: average monthly headache days, intensity, and acute medication use.
– Dystonia and spasticity: validated severity scales, range of motion, caregiver burden, and ease of hygiene.
– Hyperhidrosis: gravimetric sweat testing and patient-reported impact on daily activities.
– Overactive bladder: voiding diaries and episodes of urgency or incontinence.
Most medical uses involve periodic retreatment because nerve terminals sprout and signaling gradually returns. Dosing strategies, injection patterns, and intervals are individualized based on goals, side-effect tolerance, and response history. While many indications have strong evidence and regulatory approvals in certain regions, others remain off-label; clinicians weigh benefits and risks with patients and consider local guidelines. Importantly, botulinum toxin typically complements—not replaces—other therapies. In migraine, for example, people may continue lifestyle measures and preventive medications; in spasticity, physical and occupational therapy remain foundational. The shared objective is practical relief that translates into better days, not just improved scores on a chart.
Safety, Side Effects, Contraindications, and Choosing a Provider
Botulinum toxin is widely used with a favorable safety profile when administered by trained professionals, but no procedure is risk-free. The most common side effects are temporary and local: mild injection-site pain, small bruises, transient headaches, or a heavy feeling near treated areas. In cosmetic areas around the eyes or forehead, unintended diffusion can occasionally lead to temporary eyelid or brow droop; careful dosing and placement minimize this. For medical indications in the neck or jaw, transient chewing fatigue or neck weakness may occur. Glandular treatments can lead to dryness in nearby tissues. Systemic effects are rare at typical cosmetic doses, but patients should still understand and consent to the spectrum of possibilities.
Candidacy and precautions deserve attention. People who are pregnant or breastfeeding are generally advised to defer treatment because safety data are limited. Those with certain neuromuscular disorders (for example, myasthenia-like conditions) or significant baseline muscle weakness may be at increased risk of exaggerated effects. Some antibiotics and medications that affect neuromuscular transmission may potentiate toxin effects. A history of keloids or bleeding disorders requires planning around injection technique and bruising risk. Repeated high cumulative dosing at short intervals may increase the chance of developing neutralizing antibodies, potentially reducing effectiveness over time; spacing treatments and using the minimum effective dose can help mitigate this risk.
How to vet a provider in a crowded marketplace:
– Verify medical qualifications and specific training in facial anatomy or the relevant treatment area.
– Expect a consultation that reviews your medical history, goals, and alternatives, not just a quick sign-up.
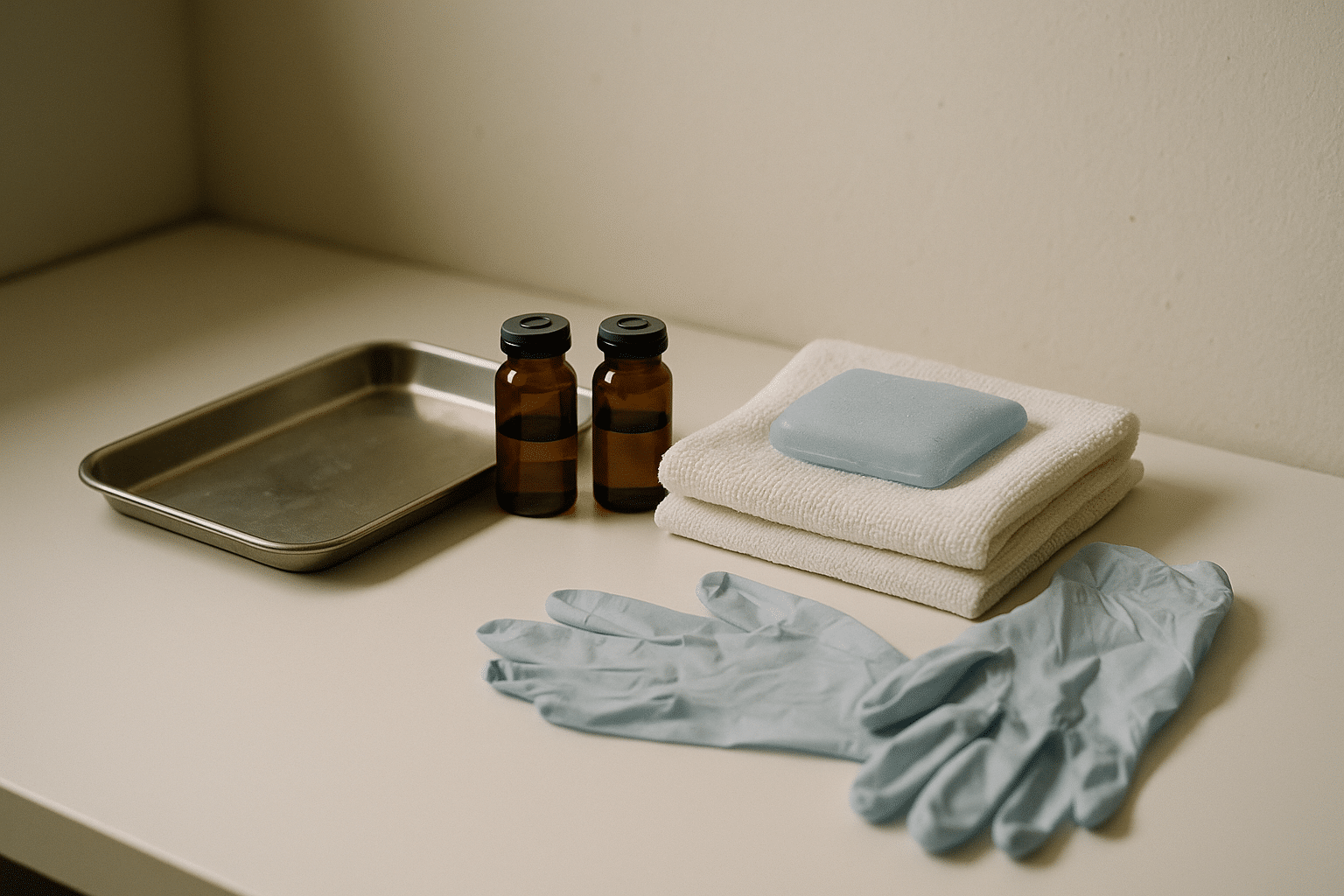
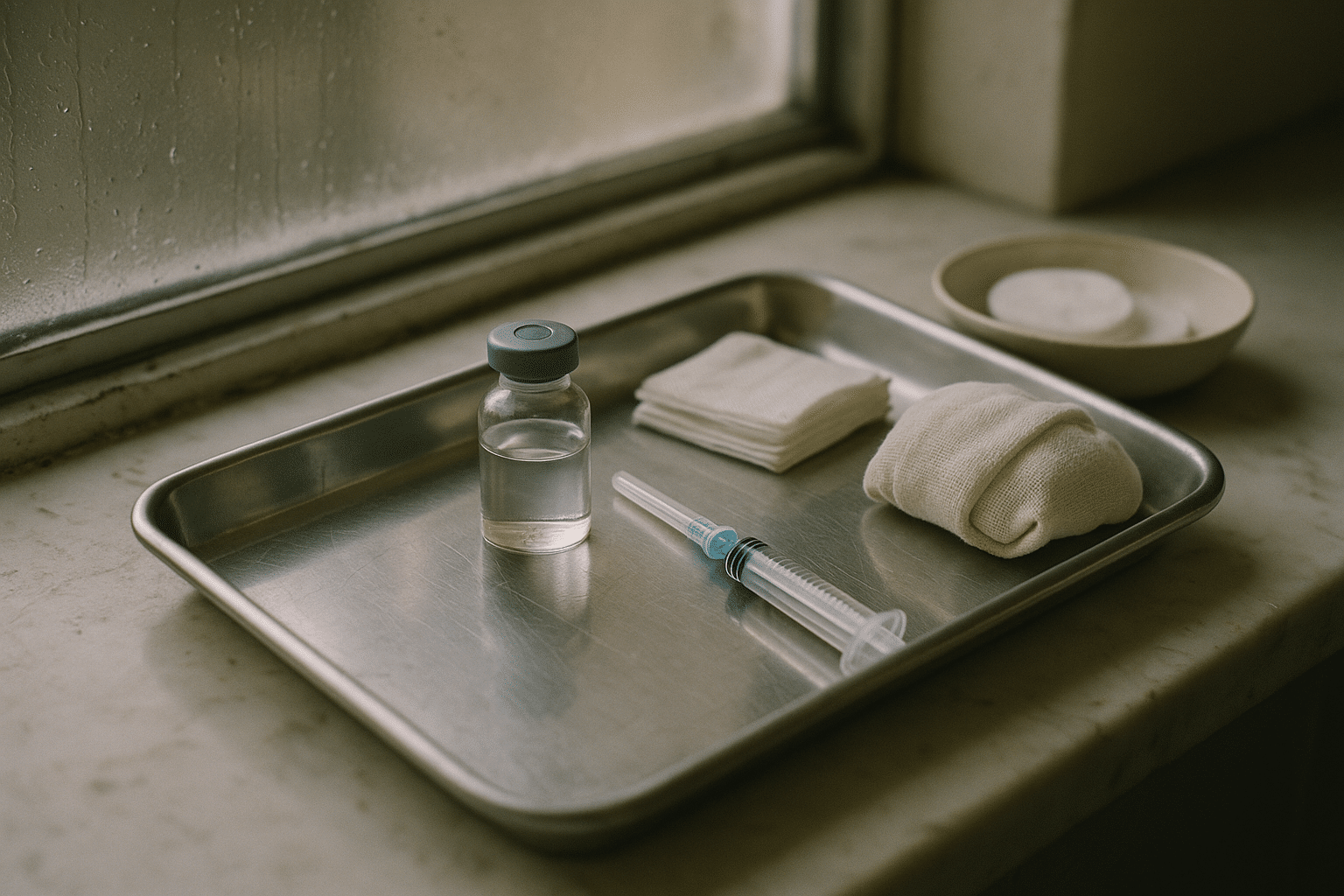
– Look for a clean, clinical environment with appropriate hygiene and emergency readiness.
– Ensure you receive informed consent documents that explain benefits, risks, and aftercare in plain language.
– Ask about follow-up policy, including how touch-ups and adverse events are handled.
Aftercare is straightforward but meaningful: avoid rubbing or massaging treated areas for several hours, keep vigorous exercise for later in the day if advised, and report unexpected changes such as asymmetry, significant weakness, or vision changes. A planned follow-up at about two weeks enables a “test, then tailor” approach, where micro-adjustments can refine balance. The end goal is not to chase maximal immobility but to achieve the specific, functional, or cosmetic outcome that feels right for you.
The Treatment Journey: Consultation, Procedure, Aftercare, and Long-Term Planning
Your experience generally unfolds in a few stages. The consultation sets the tone: you’ll discuss your medical history, what you hope to achieve, and what trade-offs you are willing to accept. Photographs and dynamic assessments (smiling, frowning, raising brows) help map injection sites. A clear plan includes targeted muscles or glands, an estimated dose range, expected onset and duration, likely side effects, and how follow-up is handled. You should leave the visit knowing exactly what will happen on procedure day and how to reach the clinic afterward.
On the day of treatment, the process is usually efficient. Skin is cleansed, and some clinicians use a cool pack or topical numbing for comfort. Injections are brief, often described as a quick pinch. Small, temporary bumps can appear at injection sites and settle within minutes to hours. Makeup, if used, is typically paused until the skin is clean and calm later that day. You can return to daily tasks quickly, though very heavy workouts or pressure on treated areas may be postponed for a short period if advised. Think of the hours after treatment as letting a snow globe settle—minimal disturbance encourages a smooth result.
Aftercare includes light movement of the treated muscles if recommended, avoiding pressure or massage over the injection sites, and monitoring for minor bruising that fades with time. A check-in around two weeks is valuable; this is when peak effect is usually reached and when small adjustments can harmonize movement across treated and untreated areas. Maintenance scheduling varies, but many people return quarterly. Over the long term, some find that consistent treatment softens the habit of forceful expression, allowing dose reductions, while others maintain a steady plan based on goals and anatomy.
Practical considerations keep expectations aligned:
– Cost varies with geography, provider expertise, and the number of areas treated; paying for quality and safety is a rational priority.
– Combination plans may pair toxin with skincare, peels, or non-invasive devices to address texture and pigment while toxin manages motion lines.
– Alternatives exist: for volume loss, fillers; for fine texture, topical retinoids and lasers; for sweat concerns, antiperspirants or device-based treatments in selected cases.
– Myths to retire: toxin does not cushion the skin permanently, it is not addictive in a pharmacologic sense, and it rarely migrates far from its target when administered correctly.
As you plan, keep your goals specific and realistic. If your objective is to look more rested on video calls, that may mean treating frown lines while preserving forehead lift. If migraines keep you from work or family time, ask your clinician whether you meet criteria for medical treatment pathways. Whatever the aim, a thoughtful, evidence-aligned approach—plus transparent follow-up—tends to deliver outcomes you can appreciate in the mirror and in your calendar.
Conclusion: Clear Expectations for Confident Decisions
Botulinum toxin treatments offer a measured way to soften motion-driven lines and to manage selected medical conditions born of muscle or gland overactivity. Their appeal comes from precision, reversibility, and the ability to tailor outcomes to your anatomy and preferences. The keys to success are candid conversations about goals, an experienced injector who understands both art and anatomy, and a plan that values safety as highly as results. With those pieces in place, you can decide if and how this treatment fits your routine, your budget, and your vision of feeling like yourself—only a bit more at ease.