Botulinum Toxin Treatments: Uses, Risks, and Aftercare Guide
Outline and How to Use This Guide
Think of this article as a map for a journey you can actually navigate. First, we outline the terrain so you know where you’re headed; then we walk each path carefully, stopping where questions usually appear. The structure is designed to move from big-picture clarity to practical detail without getting lost in jargon or hype. Here’s what we’ll cover and why it matters.
– Foundations and overview: We start with a clear roadmap of what botulinum toxin is, where it’s used (cosmetic and medical), and how this guide is organized so you can skip to the sections you need.
– How it works and who benefits: You’ll learn how the toxin blocks nerve signals to muscles and glands, with examples spanning facial lines, excessive underarm sweating, chronic migraine prevention, spasticity management, and more.
– Safety, risks, and contraindications: We detail common and uncommon side effects, who should avoid treatment or proceed cautiously, interactions that may increase risk, and how clinics mitigate issues with dose planning and anatomy-based technique.
– The treatment journey and aftercare: From pre-visit preparation and what happens in the chair to proven aftercare habits, we lay out realistic timelines for onset, peak effect, and duration, plus what to do if something feels off.
– Results, longevity, alternatives, and costs: We compare toxin to other options such as fillers, energy-based devices, skincare actives, and prescription preventives for migraine. You’ll also find guidance on training, credentials, and cost variables so you can set expectations before booking.
By the end, you’ll have a working understanding of how botulinum toxin fits into both appearance-focused and medical care plans. You’ll also gain criteria for sound decision-making: aligning your goals with the right indication, recognizing when a different modality is smarter, and communicating clearly with a qualified clinician. If a calm, evidence-informed approach is what you need, park here for a moment—then step forward with purpose.
How Botulinum Toxin Works and Where It’s Used
Botulinum toxin is a purified neurotoxin that temporarily blocks the release of acetylcholine at the neuromuscular junction and at certain autonomic nerve endings. In practical terms, this reduces targeted muscle contraction or glandular output for a limited period. Clinicians most commonly use type A formulations, while type B is reserved for select scenarios, such as certain movement disorders when type A is not suitable. The effect is localized when properly dosed and placed, with onset typically in 3–7 days, a peak around two weeks, and a duration that often spans 3–4 months for cosmetic facial lines and potentially longer for some medical indications.
Cosmetic use focuses on expression-related lines. Operators often treat the glabellar complex (the “11s” between the brows), forehead lines, and lateral canthal lines around the eyes. By dialing down muscle activity rather than immobilizing expression, skilled injectors can soften creases while preserving a natural look. Patients seeking contouring sometimes receive injections in the masseter muscles to reduce a bulky jaw angle; this can also dampen clenching intensity for some individuals who grind their teeth, though it is not a cure-all and requires careful dosing.
Medical indications are broader and supported by decades of study. Examples include cervical dystonia (involuntary neck muscle contractions), blepharospasm, hemifacial spasm, limb spasticity after stroke or in cerebral palsy, and focal spasticity in multiple sclerosis. In chronic migraine—typically defined as 15 or more headache days per month—protocolized injections across the head and neck can reduce monthly headache days over repeated cycles. For hyperhidrosis, particularly axillary sweating unresponsive to topical antiperspirants, localized injections can significantly decrease sweat production for months at a time. Other clinical uses include overactive bladder, detrusor overactivity associated with neurologic disease, and sialorrhea (excessive salivation), where reducing glandular output can improve comfort and quality of life.
What unites these indications is precision: accurate anatomical mapping, appropriate dose, and interval timing. The toxin’s effect is dose-dependent yet saturable, which is why highly experienced clinicians measure by units and tailor plans to muscle mass, baseline function, and goals. For readers comparing modalities, consider how toxin differs from alternatives: it modulates movement or secretion rather than filling volume or resurfacing skin. If your goal is smoother dynamic lines or drier underarms, that distinction matters; if you need volume restoration or texture change, other tools may be more appropriate alone or in combination.
Safety Profile, Risks, and Who Should Avoid Treatment
No medical intervention is risk-free, and botulinum toxin is no exception. The overall safety profile is well-characterized: most side effects are mild and temporary, such as localized tenderness, injection-site bruising, or a short-lived headache. Transient eyelid or brow ptosis can occur if the toxin diffuses to nearby muscles, usually resolving over weeks as the effect diminishes. When used for hyperhidrosis, some people notice compensatory sweating in untreated areas, which can be bothersome even though the original site remains drier.
Less common risks include asymmetry that requires touch-up once peak effect is visible, excessive weakening leading to a “heavy” sensation, or dry eyes if injections alter blink dynamics around the eyelids. Systemic spread of effect is rare at cosmetic and focal therapeutic doses, yet regulators emphasize vigilance for symptoms like generalized muscle weakness, difficulty swallowing, or breathing changes; such symptoms warrant prompt medical evaluation. Repeated high cumulative doses over time may increase the chance of neutralizing antibody formation, which can reduce effectiveness. This is one reason trained clinicians avoid overly frequent retreatment and plan units carefully.
Contraindications and cautions help keep treatment prudent. People with active infection at the intended injection site should defer. Individuals with certain neuromuscular disorders (for example, myasthenia gravis or Lambert–Eaton myasthenic syndrome) face elevated risk of exaggerated weakness and generally should not receive toxin unless a specialist directs care. Those who have known hypersensitivity to any component must avoid it. Pregnancy and breastfeeding are typically considered do-not-treat periods due to limited safety data. Some medications—such as aminoglycoside antibiotics or agents that affect neuromuscular transmission—may potentiate the effect, so disclosing your medication list is essential. For forehead work, pre-existing eyelid droop or very heavy brows raises the chance of unwanted changes; a conservative plan or alternative approach may be safer.
Risk reduction strategies are straightforward but meaningful: choose a clinician with substantial, relevant training; share your medical history, migraine frequency, sweating patterns, or spasticity goals; and align on conservative dosing for first-time treatments. Clear pre- and post-care instructions reduce bruising and migration risk, while measured follow-up at two weeks allows fine-tuning. Thoughtful planning turns a narrow margin for error into a comfortable lane.
The Treatment Journey and Aftercare That Actually Helps
Preparation can make the day feel calmer and the results cleaner. A pre-visit consult clarifies your goals, maps out target areas, and sets expectations on onset, peak effect, and retreatment timing. To minimize bruising, many clinics suggest avoiding alcohol for 24 hours and, with your clinician’s approval, pausing nonessential supplements known to increase bleeding risk, such as high-dose fish oil or ginkgo. If you are on prescribed anticoagulants, do not stop them without explicit guidance from your prescribing clinician; instead, plan for gentle technique and extra pressure afterward.
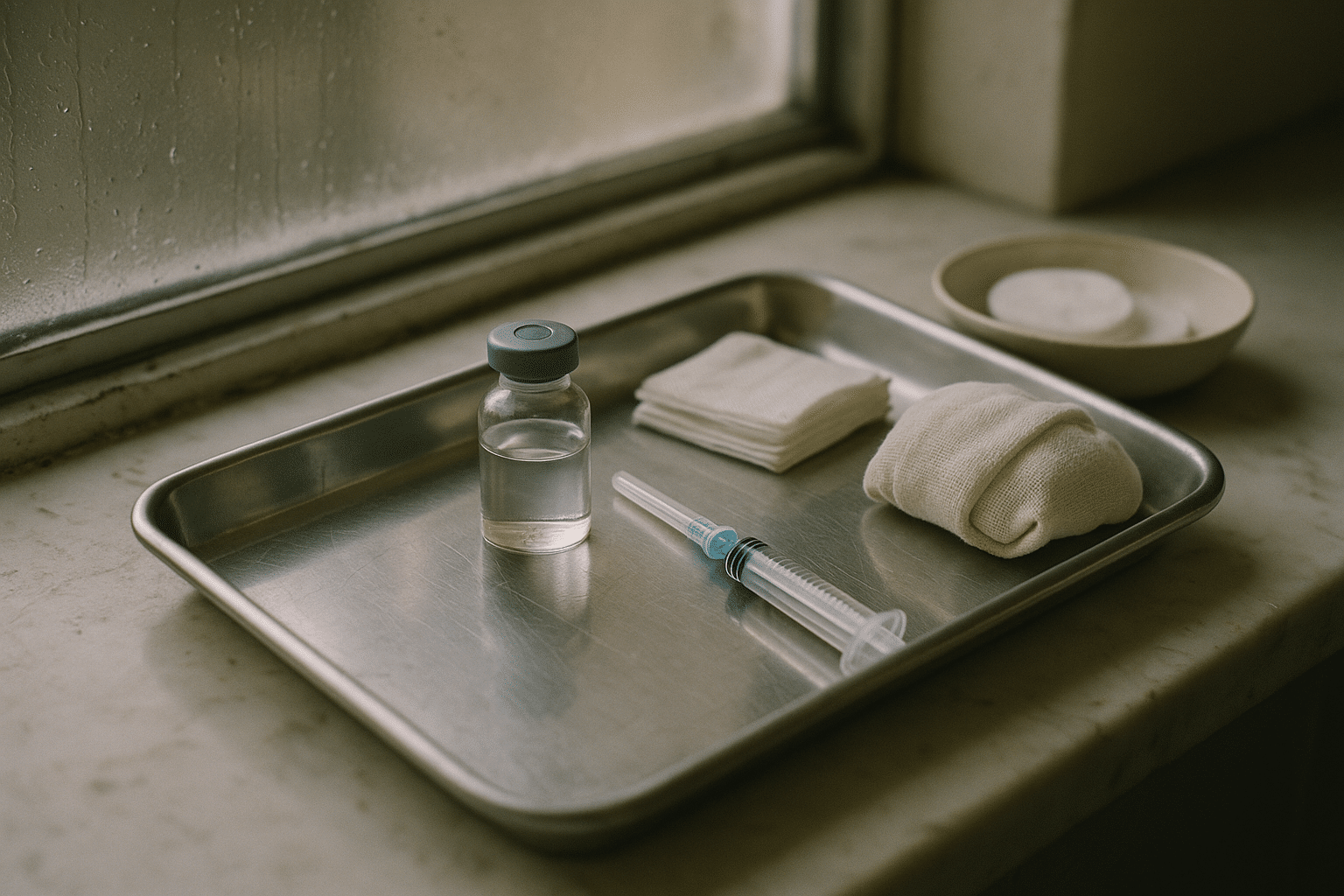
On treatment day, your provider will clean the skin, may mark landmarks, and use tiny needles to place micro-aliquots at strategic points. Most people describe the sensation as quick pinches; topical numbing is rarely required but can be used for comfort in sensitive areas or larger medical treatments. Ice or firm pressure after each injection point helps limit bruising. The visit is typically brief, though medical protocols (for migraine, spasticity, or bladder) can take longer due to the number of sites involved.
Aftercare is about smart restraint. Evidence-based guidance generally includes the following:
– Keep your head upright for several hours after treatment and avoid pressing or massaging the injected areas unless your clinician advises otherwise.
– Skip strenuous exercise, saunas, and hot yoga for the rest of the day to reduce the chance of unwanted diffusion.
– Delay facials, microcurrent devices, or aggressive skincare around the treated zones for 24–48 hours.
– If you bruise, use cool compresses intermittently during the first day; arnica or topical vitamin K may be soothing for some, although evidence is mixed.
Timeline expectations help you read your results without stress. Early changes may appear by day three, with peak effect around day 10–14. For some medical indications, meaningful improvement builds over multiple cycles spaced roughly 12 weeks apart. If an eyebrow looks uneven at day five, resist the urge to panic; the full picture arrives at the two-week mark, when adjustments can be considered. Most people return to daily routines immediately, taking only simple precautions. Should anything feel unusual—such as notable weakness outside the treated area, difficulty swallowing, or visual changes—contact your provider promptly for assessment.
Finally, create a record. Photos taken before and two weeks after help you and your clinician understand dose-response and fine-tune future plans. Jot down how long the effect lasted and how you felt at various milestones. That little logbook becomes your compass for steady, predictable outcomes.
Results, Longevity, Alternatives, and Cost Considerations
The hallmark of botulinum toxin is a smooth, subtle recalibration rather than a dramatic overnight transformation. Cosmetic results often last about 3–4 months, though intervals vary with metabolism, muscle strength, dose, and the specific area. Underarm hyperhidrosis responses can last longer—many months in some cases—because the target is glandular output rather than dynamic muscle movement. For chronic migraine, benefit commonly accumulates after two or more cycles as the nervous system’s patterning shifts; measuring headache days and severity with a simple diary can make the improvement visible.
Alternatives and complements deserve equal airtime. If your goal is volume restoration for static folds or hollowing, hyaluronic acid fillers or biostimulatory agents may be more appropriate. For surface texture and tone—think pores, fine creping, and dyschromia—modalities such as fractional lasers, radiofrequency microneedling, peels, and a consistent skincare routine with retinoids and sunscreen can play lead roles. For masseter-related clenching, night guards, physical therapy, and stress management complement toxin’s muscle-calming effect. Hyperhidrosis has non-injection options too: high-strength topical antiperspirants with aluminum salts, iontophoresis for palms/soles, oral anticholinergics in select cases, and energy-based devices designed to reduce sweat gland function. For migraine prevention, lifestyle adjustments, cognitive-behavioral strategies, magnesium in appropriate candidates, and prescription preventives—including beta-blockers, certain antidepressants, antiepileptics, and monoclonal antibodies targeting the CGRP pathway—offer a wide toolbox to personalize care.
Cost varies with geography, clinical expertise, and whether fees are calculated per unit or per area. Medical indications may be covered by insurance in some regions under specific criteria, while cosmetic goals are typically self-pay. Beyond the headline price, value depends on the thoughtfulness of the plan: precise dosing, conservative first-timer strategies, and reliable follow-up support. Choosing a provider is about more than slick photos; consider:
– Training and case volume in your indication (cosmetic lines, migraine, spasticity, or sweating).
– Willingness to discuss anatomy, risks, and alternatives without pressure.
– A clear policy for follow-up and touch-ups after the two-week mark.
– Transparent pricing and documentation of units used.
Set expectations with the same care you set a calendar reminder. Toxin is temporary by design; its reversibility is part of its appeal and a reason to plan maintenance on a schedule that suits your life. Many people alternate areas or rotate timelines to manage costs and keep outcomes steady. When goals, budget, and clinical judgment align, the result is not just smoother skin or fewer symptoms—it’s a plan you can sustain.
Conclusion: Making a Calm, Informed Decision
Botulinum toxin treatments sit at a rare intersection: a single tool with meaningful roles in both confidence-boosting aesthetics and quality-of-life medical care. The through line is precision—mapping the right targets, respecting dose, and allowing time for effect. If you are weighing smoother expressions, drier underarms, fewer headache days, or relief from troublesome muscle contractions, start by clarifying your goals, then match them to the indication with the strongest evidence. Embrace conservative beginnings, prioritize providers who educate without rushing, and commit to simple aftercare. With that approach, you give yourself room to learn how your body responds and to refine the plan over time—measured, reliable, and aligned with what matters to you.