A Practical Guide to Botulinum Toxin Treatments: Uses, Safety, and Aftercare
How This Guide Is Structured and How Botulinum Toxin Works
Outline of what you’ll learn and how to use it:
– Core concepts: what botulinum toxin is and how it temporarily relaxes muscles or reduces gland activity.
– Uses: cosmetic applications and medical indications across multiple specialties.
– Safety: common side effects, who should avoid it, and risk reduction tips.
– Procedure: consultation, injection day, and aftercare timeline.
– Decisions: pricing, provider selection, and a practical conclusion to help you move forward.
Interest in botulinum toxin has expanded quickly because it can refine expression lines and also ease symptoms in conditions linked to overactive muscles or glands. The key to making a good decision is understanding how the medication works and what it can and cannot do. This guide is educational and not a substitute for personalized medical advice. If you are considering treatment, consult a qualified clinician who can evaluate your medical history, goals, and risk profile.
Botulinum toxin is a purified neurotoxin produced by a bacterium that, when used in controlled medical doses, temporarily blocks the release of acetylcholine at neuromuscular junctions or cholinergic nerve terminals. Different serotypes exist, with type A and type B most commonly used in clinical practice. Type A typically cleaves SNAP-25, a SNARE protein crucial for neurotransmitter release, while type B targets synaptobrevin. The result is a reversible reduction in muscle contraction or glandular activity. Effects generally begin within 2–5 days, peak around 1–2 weeks, and taper over 3–4 months for cosmetic indications, though therapeutic uses can vary. Because manufacturers use different biological assays, units are not interchangeable among products.
Evidence from randomized and real-world studies supports multiple applications. Trials of botulinum toxin type A for glabellar lines have shown substantial reductions in wrinkle severity versus placebo at day 30, with high patient and evaluator satisfaction. In chronic migraine, pooled analyses report meaningful reductions in monthly headache days for a proportion of patients, often by several days, with improved quality-of-life scores. For focal spasticity and cervical dystonia, studies show improved muscle tone and function when administered by experienced injectors. In hyperhidrosis, sweat production can drop markedly after treatment. While outcomes differ by indication and individual biology, the overall signal is consistent: when performed safely and appropriately, this is a valuable tool with temporary, controllable effects.
Key takeaways at a glance:
– Onset and peak: 2–5 days to start, about 14 days to peak.
– Typical duration: roughly 3–4 months for cosmetic areas; some medical uses may last longer or require tailored intervals.
– Reversibility: the nerve terminal recovers as new synaptic machinery forms; results are not permanent.
– Individual variation: dose, placement, and metabolism influence both efficacy and duration.
Indications: Aesthetic and Medical Uses, With Realistic Expectations
Aesthetic applications focus on softening dynamic lines caused by repeated expression. Commonly treated areas include frown lines between the brows, horizontal forehead lines, and lines at the outer corners of the eyes. In some cases, carefully placed injections can refine jawline contours by reducing masseter hypertrophy, balance a “gummy” smile, or relax vertical bands in the neck. It’s important to distinguish this approach from volume-restoring procedures: botulinum toxin modulates muscle or gland activity; it does not add fullness. For many people, combining routine skincare, sun protection, and prudent toxin dosing yields fresher, more rested features without drastically altering one’s face.
Medical indications are wide-ranging and highlight the toxin’s versatility. Neurology and rehabilitation teams use it to manage focal spasticity after stroke, brain injury, or in conditions such as multiple sclerosis; precise dosing can reduce involuntary contractions and improve function alongside therapy. Ophthalmology applies it for blepharospasm to calm eyelid spasms. In movement disorders like cervical dystonia, targeted injections can reduce painful neck contractions. Urology employs it for overactive bladder to lower urgency and incontinence episodes. Dermatology and neurology collaborate on hyperhidrosis, where reducing cholinergic input to sweat glands significantly limits sweating in the underarms, palms, or soles. Sialorrhea (excessive drooling) can also be addressed by treating salivary glands; by moderating secretion, chewing, swallowing, and social comfort may improve.
Expectations should be clear and conservative. Many cosmetic patients notice visible softening rather than complete erasure of lines, particularly at rest. Functional gains in medical indications depend on anatomy, dosing, and adjunct therapies. Some examples reported in the literature:
– Chronic migraine: a meaningful subset sees several fewer headache days per month.
– Hyperhidrosis: sweat reduction can be dramatic in responders, often improving daily comfort and wardrobe choices.
– Spasticity: tone reduction can facilitate hygiene, stretching, and task performance when integrated with rehabilitation.
Not everyone is an ideal candidate. A candid pre-treatment conversation should include:
– Your goals: subtle refresh versus stronger muscle relaxation.
– Medical history: neuromuscular conditions, prior surgeries, and medication list.
– Lifestyle needs: performance demands, athletic schedules, and work considerations.
– Maintenance planning: willingness to return at intervals to sustain results.
Because different formulations use distinct biological assays, dosing guidance is product-specific; units cannot be compared across brands. Providers tailor placement and dose to minimize diffusion where unwanted (for example, avoiding brow drop during forehead treatments) and to match the functional aim (such as balancing opposing muscle groups in the neck). Setting measured goals, tracking outcomes with photos, and adjusting gradually over successive sessions often provide the most natural, satisfying results.
Safety Profile, Contraindications, Side Effects, and Common Myths
When performed by trained clinicians in appropriate settings, botulinum toxin has a well-characterized safety profile. Most adverse effects are temporary and localized. The most frequently reported issues include minor bruising, tenderness, swelling at injection sites, and transient headache. A small percentage may experience eyelid or brow heaviness if product diffuses into nearby muscles, typically resolving as the effect wanes. Asymmetry can occur if one side responds differently; this is usually managed with conservative touch-ups once the initial dose has settled.
Less common but important events include neck weakness, dry mouth, or difficulty swallowing when treating certain regions, especially in therapeutic doses for cervical dystonia or sialorrhea. Systemic symptoms are rare at cosmetic doses but can occur, particularly with higher cumulative dosing or in susceptible individuals. Prescription neurotoxin products carry a boxed warning regarding the potential for distant spread of effect; while uncommon, this underscores the need for careful patient selection, precise dosing, and prompt follow-up if unexpected symptoms arise. Immediate medical attention is warranted if swallowing, breathing, or generalized weakness problems develop.
Contraindications and cautions to discuss with your clinician:
– Active infection or skin inflammation at planned injection sites.
– Known hypersensitivity to components in the formulation.
– Neuromuscular junction disorders (for example, myasthenia gravis or Lambert–Eaton syndrome), which can increase susceptibility.
– Pregnancy and breastfeeding: treatment is generally deferred due to limited safety data.
– Concomitant medications that may potentiate effect (for example, certain antibiotics or muscle relaxants); bring a complete list of prescriptions and supplements.
Myths to reconsider:
– “It freezes your face.” Goal-directed dosing aims to soften overactive lines while preserving expression. An experienced injector can prioritize natural movement.
– “Wrinkles come back worse.” As the effect fades, muscles gradually regain function; skin typically returns to baseline. Ongoing sun care and skincare influence long-term appearance far more than a single session.
– “It’s addictive.” There is no physiological dependence; repeated use reflects personal preference for maintained results.
– “Only for cosmetic use.” The medical applications span pain, muscle tone, and glandular conditions, extending benefits well beyond aesthetics.
Risk reduction tips:
– Choose qualified medical professionals who prioritize anatomy, conservative dosing, and sterile technique.
– Share your full medical history and goals; ask about diffusion risk and how asymmetry would be handled.
– Schedule follow-up for assessment around the two-week mark, when effects are near peak and subtle adjustments can be considered.
From Consultation to Aftercare: What to Expect at Each Step
A thoughtful journey begins with consultation. Your clinician will review your medical history, prior procedures, medications, and photos, then examine anatomy in motion to map muscular patterns or gland locations. Clear goals matter: a softer frown with retained brow mobility requires different placement than a stronger relaxation for frequent tension headaches. You should receive information about benefits, risks, alternatives, and expected timelines, along with an opportunity to ask questions.
Preparation can make the day smoother:
– Avoid alcohol and, if approved by your clinician, consider pausing nonessential blood-thinning supplements (for example, high-dose fish oil) a few days prior to reduce bruising risk.
– Continue essential medications unless advised otherwise by your prescribing clinician.
– Arrive with clean skin; skip retinoids and exfoliation the night before if you’re prone to irritation.
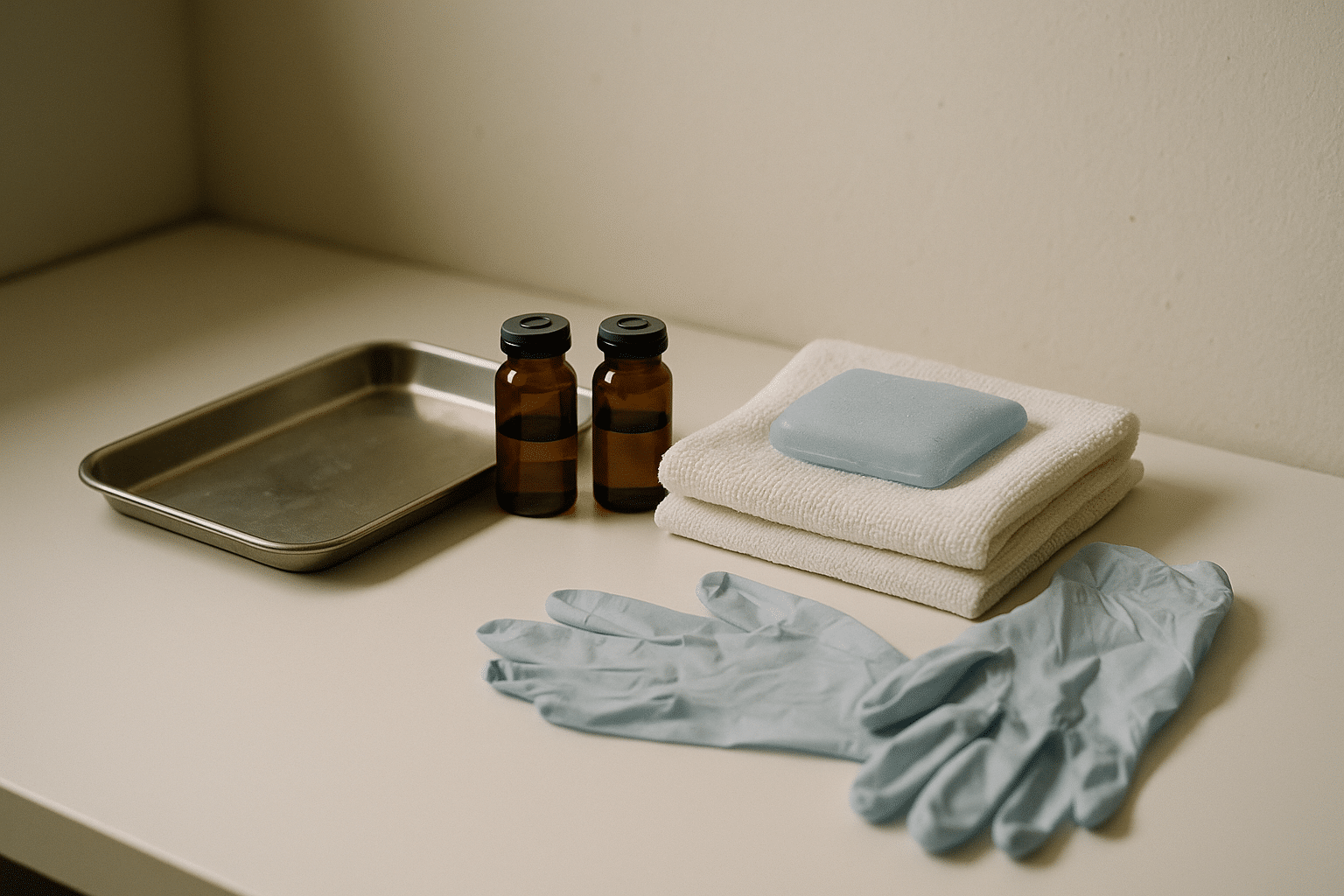
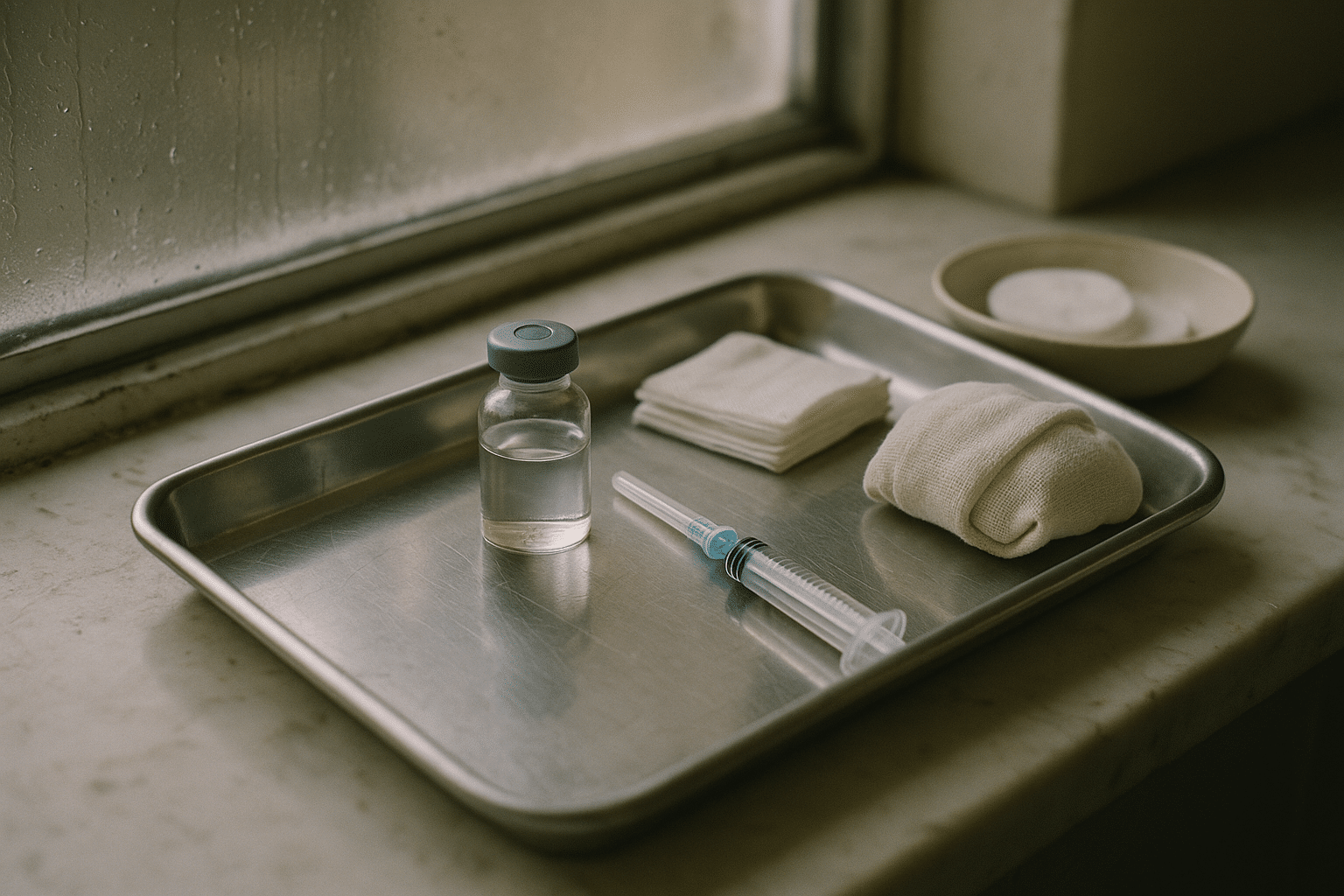
During the appointment, the area is cleansed and, if needed, topical numbing or ice is used. The injections themselves feel like quick pinches; many sessions finish in 10–20 minutes depending on the number of areas. Your clinician may ask you to contract muscles so that landmarks are easy to identify. Expect small blebs or dots that settle quickly. For medical indications, mapping may be more detailed, sometimes guided by palpation, ultrasound, or electromyography to improve accuracy in deeper or spastic muscles.
Aftercare focuses on minimizing spread and bruising:
– Stay upright for several hours; avoid pressing, massaging, or sleeping on the treated area the first night.
– Skip high-heat environments (sauna, hot yoga) and vigorous workouts for the first 24 hours.
– Use gentle cold compresses for swelling; arnica or bromelain, if approved by your clinician, may help bruising.
– Delay facials, exfoliation, or micro-needling for at least several days.
Timeline and follow-up:
– Onset often appears by day 2–5; some areas respond sooner than others.
– Full effect is typically observed around day 14; this is the ideal time for assessment.
– Duration varies by dose, muscle size, metabolism, and indication; plan for maintenance every 3–4 months in many cosmetic cases, with therapeutic intervals tailored to function and safety.
Documenting your experience helps with fine-tuning. Consider:
– Taking standardized photos at baseline, day 14, and monthly thereafter.
– Noting symptom diaries for medical indications (headaches, spasm frequency, sweat episodes).
– Discussing what felt ideal versus too strong or too light, so your plan evolves toward your preferred balance of movement and smoothness.
Choosing Wisely: Costs, Provider Selection, and Conclusion for Readers
Prices vary widely, and understanding the structure helps you compare fairly. Clinics may charge per unit or per area. Per-unit pricing aligns cost with dose, which can be helpful when tailoring subtle or asymmetric needs; per-area pricing offers predictability, though it can mask dose differences. Regional economics, clinician experience, and clinical setting influence fees. Medical indications sometimes involve higher total doses and may be billed differently than aesthetic sessions. Remember that lower price does not always equal better value; precision, safety, and follow-up support are integral to a satisfactory outcome.
Budget and value tips:
– Ask whether pricing is per unit or per area, and what range of units is typically used for your goals.
– Confirm what is included: consultation, photos, follow-up, and potential touch-up policies.
– Plan on maintenance; map out an annual schedule to avoid surprise expenses.
– Be wary of unusually low prices, rushed consults, or vague explanations about product, dosing, or aftercare.
Choosing a provider is central to results and safety. Look for clinicians with relevant medical training and ongoing education in facial anatomy or the targeted therapeutic system. A strong consultation feels collaborative, with honest discussion of benefits and limits, and readiness to say “not today” when expectations or timing aren’t right. Informed consent, sterile technique, and documented dosing maps signal professionalism. Ask what complications they’ve managed, how they would handle asymmetry, and when they schedule reassessments.
Practical red flags:
– Pressure to buy more than you planned or to treat areas you did not raise.
– Guarantees of permanent results or claims that sound too good to be true.
– No clear policy for follow-up, complications, or after-hours concerns.
Conclusion for readers: If you’re considering botulinum toxin to refresh expression or address issues like headaches, spasticity, sweating, or bladder urgency, approach it like any meaningful health decision—get informed, set measured goals, and prioritize safety. Start with a thorough consultation, bring your full medical history, and discuss a trial period of one or two cycles to calibrate dose and placement. Track your results with photos and symptom notes, then adjust incrementally. With realistic expectations and a qualified provider, treatment can be a precise, time-limited tool that supports comfort, confidence, and function without overpromising or overcorrecting.